Mosquitos and ticks thrive during the summer months, which is when they also present their greatest threat to public health. Dr. Syra Madad, Chief Biopreparedness Officer with NYC Health + Hospitals, offers advice on how to protect yourself, your family, and your pets from these disease-carrying insects.
Published August 8, 2024
By Syra Madad, D.H.Sc., M.Sc., MCP, CHEP

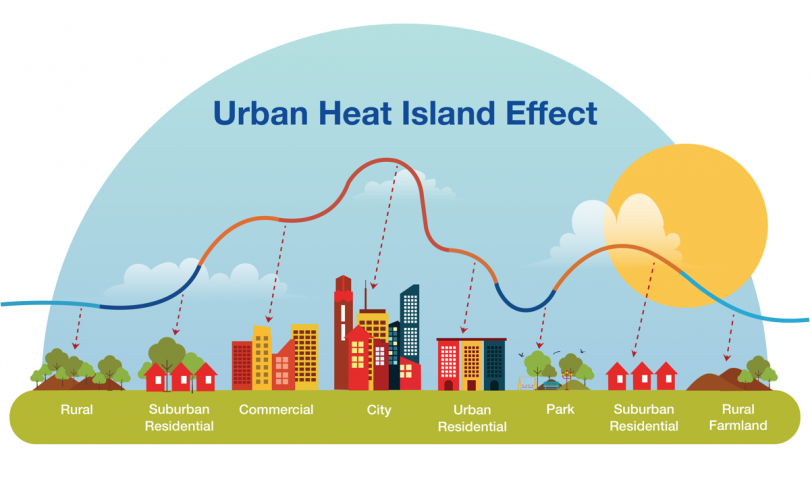
The rise in mosquito-borne and tick-borne illnesses is a pressing public health concern. In recent years, there has been a significant increase in these illnesses globally, including in the United States. Both mosquito and tick-borne diseases thrive in the summer months due to warmer temperatures and increased humidity, which create ideal breeding conditions for mosquitoes and enhanced tick activity.
The increase in diseases such as dengue, West Nile virus, and Lyme disease underscores the urgent need for effective prevention and public awareness. By adopting the ABCDE approach and taking practical preventive measures, we can combat the spread of these diseases and protect our health.
The Growing Burden of Mosquito-Borne Diseases
Dengue is a mosquito-borne viral infection that has reached unprecedented levels in the Americas, with over 9.7 million cases reported in the first half of 2024 alone, a significant rise from previous years. Symptoms of dengue include high fever, severe headache, pain behind the eyes, joint and muscle pain, rash, and mild bleeding. The CDC has issued a health advisory highlighting the increased risk of dengue in the United States, particularly in Puerto Rico and among travelers returning from endemic areas. Majority of dengue virus cases are asymptomatic, with about one in four people infected with dengue getting sick.
West Nile virus, another mosquito-borne disease, has also been detected early and extensively. For example, in New York City, there were 325 positive mosquito pools reported as of mid-2024. There’s been 103 human diseases cases including 68 neuroinvasive disease cases of West Nile virus across 26 states in 2024 so far. An estimated 70-80% of human West Nile virus infections are subclinical or asymptomatic.
Symptoms of West Nile virus infection can range from mild, flu-like symptoms to severe neurological illness. Less than 1% of infected individuals develop West Nile Neuroinvasive Disease (WNND), which typically presents as meningitis, encephalitis, or acute flaccid paralysis. People over 60 years of age, or those with certain medical conditions or undergoing treatments that cause immunosuppression—such as diabetes, hypertension, cancer, or organ transplantation—are at greater risk of developing WNND.

Image by Centers for Disease Control and Prevention via Fairfax County/Flickr. Licensed via CC BY-ND 2.0. No changes were made to the original work.
Tick-Borne Diseases on the Rise
Ticks are responsible for transmitting various diseases, with Lyme disease being the most prevalent in the United States. The blacklegged tick, which carries Lyme disease, anaplasmosis, and babesiosis, has expanded its range due to climate change, leading to increased cases even in urban areas like Staten Island and the Bronx. Symptoms of Lyme disease include fever, headache, fatigue, and a characteristic skin rash called erythema migrans. If left untreated, the infection can spread to the joints, heart, and nervous system. The warming climate has extended the tick season, allowing these vectors to remain active for longer periods and spread more widely.
ABCDE Approach to Mosquito and Tick-borne Disease Prevention:
To protect yourself against mosquito and tick-borne diseases, utilize the ABCDE approach:

- Avoid: Avoid areas with high mosquito and tick activity, especially during peak seasons. This includes wooded, brushy, and grassy areas where ticks are common, and areas with stagnant water where mosquitoes breed. Mosquitoes that carry West Nile virus usually bite around dusk and dawn.
- Block: Use Environmental Protection Agency-approved insect repellents on exposed skin and clothing. DEET, picaridin, and oil of lemon eucalyptus are effective options.
- Control: Use air conditioning and window screens to prevent mosquito entry. Regularly empty containers that collect water to reduce mosquito breeding sites.
- Dress: When outdoors, especially in wooded or grassy areas, wear long sleeves, long pants, and socks. Light-colored clothing makes it easier to spot ticks.
- Examine: After spending time outdoors, perform thorough tick checks on yourself, children, and pets. Promptly remove any attached ticks with fine-tipped tweezers.
Stay connected with Dr. Madad:
Instagram
Twitter/X
LinkedIn
Facebook