Exploring a New Chapter in Biopreparedness
The U.S. Department of Health and Human Services’ new Portable Biocontainment Unit will enhance national special pathogen response.
Published August 26, 2025
By Syra Madad, D.H.Sc., M.Sc., MCP, CHEP; Erfan Karim, MPH, Laura Hillard; Jory Guttsman; Vikramjit Mukherjee, MD

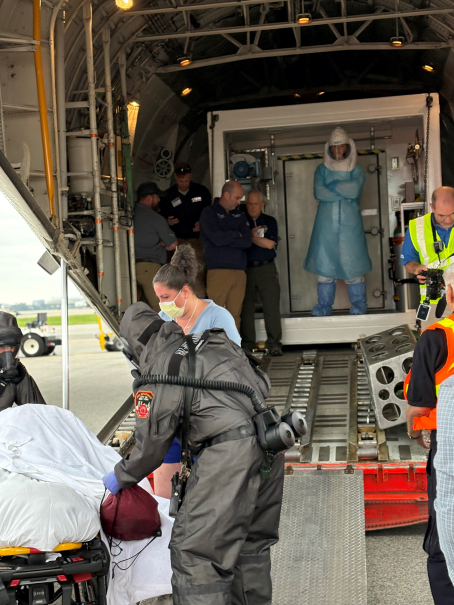
This past June, the United States reached a major milestone in national health security. The Tranquil Passport exercise, the largest special pathogen patient movement drill in U.S. history, successfully tested the new Portable Biocontainment Unit (PBCU), the first domestic capability designed for the safe medical transport of patients with high consequence infectious diseases (HCIDs), such as Ebola Virus Disease or Marburg Virus Disease.
The PBCU is not just another tool; it represents a strategic breakthrough in national biopreparedness.
Exercise Overview
The four-day exercise brought together more than 50 federal, state, local, and international partners. The scenario simulated the movement and medical care of HCID patients emerging during the 2026 FIFA World Cup. Patient actors were transported from Toronto to Regional Emerging Special Pathogen Treatment Centers (RESPTCs) in New York, Washington, D.C., Baltimore, Atlanta, and Chapel Hill.
The PBCU’s performance and simulated care inside the unit during the exercise affirmed its value as a transformative asset for special pathogens preparedness providing seamless patient isolation and supporting care and protection of health care providers during long distance international and domestic air and ground transport.
As part of this exercise, two of the authors (Syra Madad and Erfan Karim), were on the ground at LaGuardia Airport in New York City to observe firsthand the air transport operations and patient handoff to Emergency Medical Services (EMS) teams. They also had the opportunity to tour the PBCU, gaining direct insight into its functionality, safety features, and the critical role it will play in bridging national preparedness gaps.
Closing a Critical Capability Gap

The 2014 Ebola outbreak exposed gaps in the nation’s ability to transport patients suspected of or confirmed with high consequence infectious diseases. While several American healthcare workers were successfully evacuated from West Africa using improvised biocontainment methods, these missions required extraordinary coordination and highlighted our lack of standardized domestic transport capability. The nation continues to face several limitations for transporting patients domestically over long distances. EMS providers face time constraints on the duration in which they can provide care in the cumbersome Personal Protective Equipment (PPE) required for these types of transfers, complicating ground transport options over long distances.
For air transport, the nation relied on a single vendor for all international and domestic HCID transports, exposing the system to potential risks in the event that multiple patients required simultaneous transport. With only 13 RESPTCs in the entire United States, these transport limitations complicate the ability to get patients from many areas to definitive care.
Now, the PBCU is one method to help fill that gap. Built to move up to 10 seated or two stretcher patients under biocontainment precautions, it features HEPA filtration, negative pressure, continuous patient monitoring, advanced critical care capabilities and easy to disinfect surfaces. It integrates with C130 and L100 aircraft or can be deployed by ground using a 53-foot trailer. For the first time, the U.S. has the means to transport clusters of patients safely, protecting healthcare workers and communities alike.
Embedding Capability in a National System
The success of Tranquil Passport extends beyond testing a single asset, it demonstrated how the PBCU fits within the broader National Special Pathogen System (NSPS). This system is a tiered network of health care facilities, transport systems, and public health partners guided by NETEC’s national strategy, which emphasizes coordination, workforce readiness, sustainable infrastructure, and equity in access to care.
The PBCU is central to this system, supporting a cohesive network that spans NSPS Levels 1 through 4 health care facilities. At its core, the system ensures the safe transportation of patients from one facility to a higher level of care.
The NSPS levels include:
- Level 1: Regional Treatment Centers or RESPTCs – Level 1 facilities serve as definitive care centers and regional resource hubs, providing highly specialized care for patients suspected of or infected with a special pathogen. They also provide subject matter expertise to support all facilities within their region.
- Level 2: Special Pathogen Treatment Centers (SPTCs) – These facilities have the capacity to deliver specialized care to patients suspected of or infected with a special pathogen and serve as the primary centers for patient care delivery.
- Level 3: Assessment Centers – Widely accessible facilities that can conduct limited laboratory testing, isolate and stabilize patients, and coordinate rapid transfer to a Level 1 or 2 facility.
- Level 4: All Other Healthcare Facilities – These facilities can identify, isolate, inform, and initiate stabilizing medical care; protect staff; and arrange timely patient transport while minimizing disruption to normal operations.
WATCH: https://www.instagram.com/reel/DLYnFINsYQT/?utm_source=ig_web_copy_link&igsh=MzRlODBiNWFlZA==
A Decade of Experience
This system of care is coordinated by NETEC, a consortium of the three hospitals that successfully treated Ebola patients in the United States in 2014: Emory University Medical Center in Atlanta, NYC Health + Hospitals/Bellevue in New York City, and the University of Nebraska Medical Center in Omaha. Since its founding, NETEC has built a decade of experience in advancing U.S. preparedness for HCIDs and now serves as the congressionally approved Coordinating Body for the NSPS.
The NSPS places strong emphasis on interfacility transport, supply chain resilience, equity, and continuous workforce training. By integrating the PBCU into patient movement, the U.S. Department of Health & Human Services (HHS) ensures that appropriate air and ground transport is available to support the safe and successful transfer of HCID patients. More than just hardware, the PBCU represents a shift in mindset, from ad hoc preparedness to an integrated national infrastructure with adaptable resources for any region. As the Tranquil Passport exercise demonstrated, this work is not theoretical; it is happening in practice.
Why It Matters Today

The PBCU is more than a technological innovation, it represents a shift in mindset. Outbreaks are no longer rare or isolated events; in our interconnected world, they are a certainty and pose a direct threat to national security. Whether confronting Ebola, a novel viral hemorrhagic fever, or future unknown pathogens, we must plan, train, and rehearse for these eventualities.
The Tranquil Passport Exercise demonstrated that we are capable, but capability must be paired with sustained commitment. This includes continuous funding, regular exercises, and the ongoing maintenance of critical infrastructure. The NSPS strategy provides this framework, spanning Levels 1 through 4 health care facilities, and emphasizing workforce training, supply chain readiness, and system evaluation.
We must ensure that the readiness demonstrated during Tranquil Passport is not a singular achievement, but the standard for the nation’s response to high consequence infectious diseases. Continued investment will be essential to strengthen the National Special Pathogen System, but with the PBCU, the United States has opened a new chapter, one where our communities are better prepared to withstand and respond to special pathogen threats.
Acknowledgements
We extend our gratitude to Rick Hunt, MD, FACEP, Joe Lamana, and the entire E2A2 Exercise Team at the Center for Preparedness, Office of Planning and Exercises, Division of Exercises, Evaluations, and After-Actions (E2A2) at the Administration for Strategic Preparedness and Response, U.S. Department of Health and Human Services.
Stay Connected with Dr. Madad:
Instagram
Twitter/X
LinkedIn
Facebook
