Understanding Potential Treatments for Liposarcoma
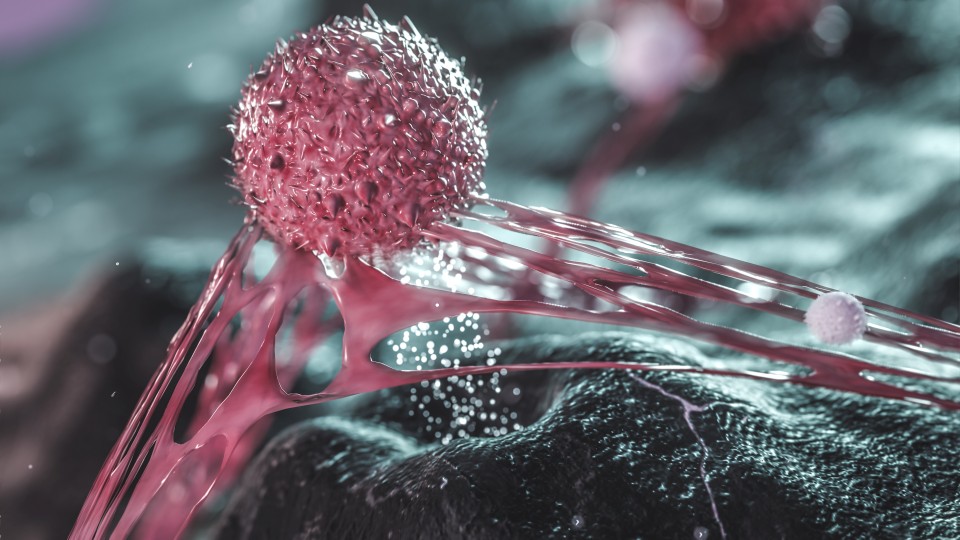
Liposarcoma is a rare type of cancer that originates in fat tissue. New methods show potential for treating this deadly disease.
Published February 12, 2026
Unfortunately, liposarcoma is generally resistant to standard treatment options, such as radiation and chemotherapy, making surgery the primary treatment method. Most cases have extra copies of the gene, CDK4, leading to excessive cancer cell division and tumor progression.
An active area of investigation is determining whether CDK4/6 inhibitors are effective at treating liposarcoma. Unlike chemotherapy or radiation, which inflict widespread DNA damage, CDK4/6 inhibitors are a newer class of drugs that work more precisely. They act like a guided missile, targeting only cancer cells that have overactive CDK4, rather than a bomb that indiscriminately affects both cancer and normal cells.
Clinical trials have shown promise, with CDK4/6 inhibitors delaying cancer progression in patients. However, it is unclear how long term CDK4/6 inhibitor treatment affects changes the molecular profile of cancer cells. These changes determine whether patients continue to respond well to therapy and survive longer or eventually acquire untreatable drug-resistant cancer.
Potential Targets for Additional Drugs
We hypothesize that CDK4/6 inhibitors and chemotherapy cause cancer cells to make different decisions over time, due to their differences in how they stop cancer growth. To test this hypothesis, we identified the genes that become activated by long-term drug treatment by CDK4/6 inhibitors or chemotherapy. We also characterized non-genetic modifications in the genome that may drive gene activation without altering the underlying DNA sequence. These modifications may represent potential targets for additional drugs that could be combined with CDK4/6 inhibitors to more effectively eliminate cancer cells.
Our research shows that while CDK4/6 inhibitors and chemotherapy affect cancer cells differently at first, over time they elicit some of the same harmful changes. In early treatment, CDK4/6 inhibitors do not turn on genes linked to inflammation and tumor growth that are immediately turned by chemotherapy. By increasing the duration of treatment beyond what is typically studied, we show that CDK4/6 inhibitors eventually activate the same harmful genes as chemotherapy—just more slowly. This is a paradigm shift in the way we think about the clinical implications of CDK4/6 treatment.
These findings change how we think about targeted treatments. While CDK4/6 inhibitors may offer initial benefits over traditional chemotherapy, cancer cells adapt to therapeutic pressure over time by increasing inflammation to enhance their survival. Understanding this process allows for researchers to find new opportunities to intervene. Adding medications that prevent drug-resistance mechanisms in combination with CDK4/6 treatment are possible solutions to improving long-term patient outcomes, especially as new targeted therapies enter the clinic.
A detailed scientific version of this work is available as a preprint on bioRxiv.
Also read: Advancing Cancer Research and Therapies