Nutrition Modeling Consortium
Through a grant provided by the Bill & Melinda Gates Foundation, The New York Academy of Sciences created a consortium for nutrition modeling aimed at improving the usability of tools for nutrition policy making and at increasing their uptake by low middle income countries (LMIC). In April 2017, the Institute partnered with the Micronutrient Forum to convene a two-day technical consultation to review seven tools designed to help decision makers in LMICs develop and streamline their nutrition programs and interventions.
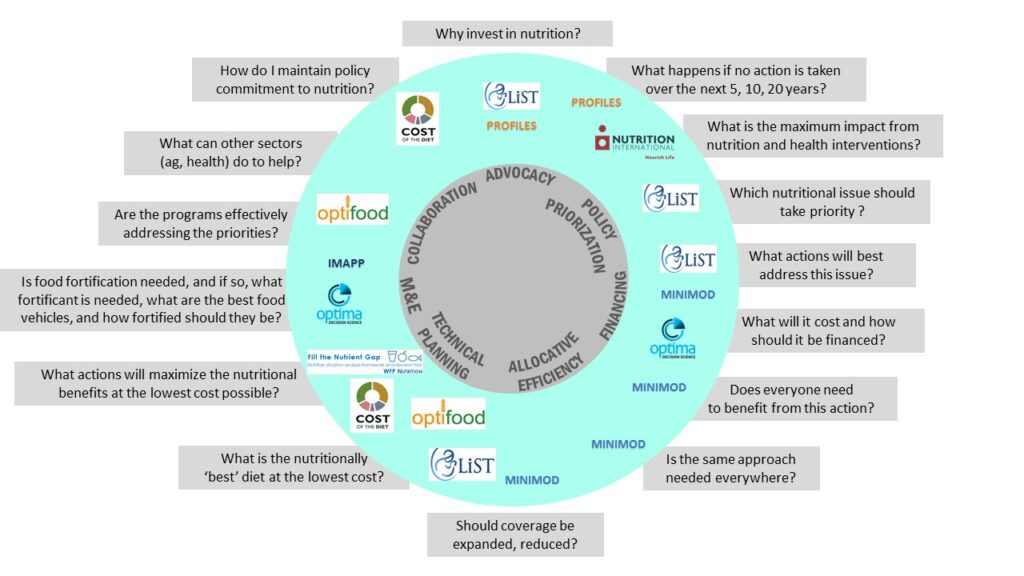
These tools were selected on the basis of their ability to elaborate nutrition policy scenarios adapted to national priorities and contexts, whether through the use of mathematical optimization routines or other evidence-based analytical approaches. Services provided by those tools range from advocacy to allocative efficiency to budget planning. The meeting highlighted the deep capabilities of those tools, and several examples were presented of successful use that confirmed their potential utility to nutrition policy making.
What is Nutrition Modeling?
Nutrition Modeling refers to computer assisted optimization routines that seek to select a best solution with regard to a nutrition objective among a set of available policy or program alternatives. Some tools on the Consortium follow mathematical optimization algorithms, some use spreadsheet formula, some use qualitative methods to drill down on nutrition data. Regardless of design, they all share the intent of improving the use of available knowledge and data in designing nutrition policies and programs.
The mandate of the Nutrition Modeling Consortium is to:
- Increase end-users’ input in the specification of services to be provided by these tools.
- Help end-users understand better how those tool can serve their nutrition programming needs.
- Advance the joint utility and effectiveness of the modeling tools through a collective effort by nutrition modelers in order to enhance their technical inter-operability, and improve their usability to end-users.
How the Consortium Works
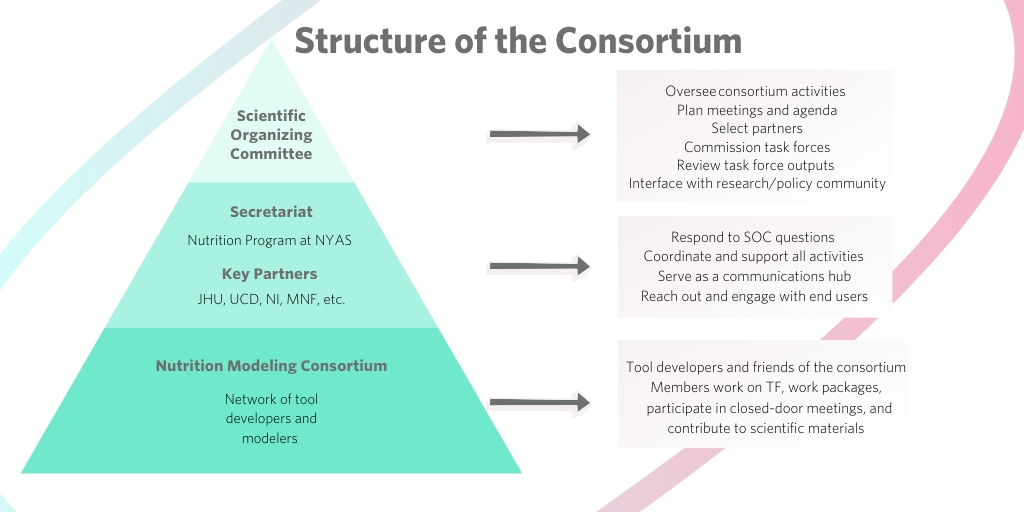
The Consortium of Nutrition Modelers aims to improve the use of the evidence base in policy and program decision making through the use of mathematical modeling of nutrition activities. It is led by a Scientific Organizing committee composed of nutrition modelers and end-users. The Secretariat has the responsibility of linking the SOC to the modeling community and to end-users, to coordinate the work of the Consortium and to organize and convene meetings of the Consortium.

Contact Us
To learn more about the Nutrition Modeling Consortium, contact us at nutrition@nyas.org.