Public health expert Dr. Syra Madad reflects on resilience, innovation, and collaboration she saw in 2024, though gaps remain in equity, healthcare worker safety, and public trust in science.
Published January 7, 2025
By Syra Madad, D.H.Sc., M.Sc., MCP, CHEP
As we step into 2025, I reflect on the remarkable progress and challenges of 2024 in the field of special pathogens and public health. From the rapid containment of the Marburg virus in Rwanda to groundbreaking strides in global health in disease elimination, the year was a testament to resilience, innovation, and collaboration. These achievements emerged against a backdrop of formidable challenges, including zoonotic threats like H5N1, the ongoing Mpox Clade 1 outbreak, and the persistent decline in vaccination rates in the United States. Yet, the collective response—driven by scientific advances, decisive leadership, and community engagement—offers a roadmap for tackling future health crises with resolve and ingenuity.
While these milestones provide reasons for optimism, they also underscore the gaps that remain in equity, healthcare worker safety, and public trust in science. The lessons of 2024 reaffirm the critical need for vigilance, preparation, and global solidarity. Here are five key achievements that exemplify the progress we’ve made and the challenges we must continue to address.
1. Marburg Outbreak Response: A Triumph of Speed and Coordination
The 2024 Marburg virus outbreak in Rwanda stands as a benchmark for swift and effective epidemic response. Historically linked with fatality rates as high as 88%, this outbreak achieved an unprecedented case fatality rate of 22.7% thanks to Rwanda’s rapid and coordinated efforts. Within nine days of the outbreak’s declaration, the country launched a vaccine trial, administering over 1,600 doses of the investigational Sabin chAD3 MARV vaccine to healthcare workers—who accounted for nearly 80% of confirmed cases—and other at-risk groups.
The early deployment of experimental therapeutics, such as Remdesivir and monoclonal antibodies, combined with advanced supportive care, saved lives and reduced the outbreak’s severity. Rwanda’s decisive actions underscore the importance of rapid intervention, effective surveillance, and the availability of experimental countermeasures, offering a critical template for managing future high-consequence infectious diseases.
Despite its success, the outbreak highlighted critical challenges, particularly the vulnerability of healthcare workers. In the realm of special pathogens and high-consequence infectious diseases—a field in which I work closely—healthcare worker infections are considered a “never event”—an occurrence that should never happen. As a professional dedicated to preparedness and response in this critical area, I understand firsthand that allowing frontline responders to contract infections while caring for patients signals systemic failures in multiple areas, including infection prevention protocols, administrative controls to ensure safe working environments, and clear, consistent healthcare worker guidance to mitigate exposure risks.
In Rwanda, nosocomial transmission during the Marburg outbreak, compounded by delays in diagnosis, led to unacceptably high infection rates among healthcare workers. This underscores the urgent need for robust infection prevention and control (IPC) measures, surveillance and screening systems, comprehensive training programs, and accessible mental health support to protect frontline healthcare workers. In a co-authored article, “Protecting Healthcare Workers: A Vital Imperative in Rwanda’s Marburg Virus Outbreak and Beyond,” we outlined actionable strategies to strengthen protections for frontline responders during outbreaks. Safeguarding healthcare workers is not just a moral imperative but a foundational requirement for effective epidemic response and resilience in future crises.
2. Significant Milestones in Global Health
The year 2024 witnessed remarkable successes in global health, underscoring the power of collaboration. Among the most notable achievements were strides in disease elimination, with countries like Egypt and Cabo Verde being declared malaria-free after decades of effort. Seven nations, including Brazil, Pakistan, and Chad, eliminated neglected tropical diseases, while Guinea achieved maternal and neonatal tetanus elimination. In the Americas, measles-free status was reverified, and several countries made strides in halting mother-to-child transmission of HIV and syphilis. These accomplishments are a testament to sustained partnerships, robust public health systems, and the collective dedication to improving quality of life worldwide.
Progress was also made in tackling noncommunicable diseases (NCDs) and mental health, with a renewed emphasis on prevention and control. WHO’s 2024 reports highlighted significant declines in tobacco use and a 38% global reduction in drowning deaths since 2000. However, the growing burden of conditions like obesity, diabetes, and neurological diseases underscored the need for innovative strategies and equity in healthcare access. On the global stage, leaders addressed critical health priorities, including antimicrobial resistance and the intersection of climate change and health, while advancing negotiations on pandemic preparedness agreements. These milestones highlight a year of transformative progress in global health!
3. Addressing the Growing Threat of H5N1
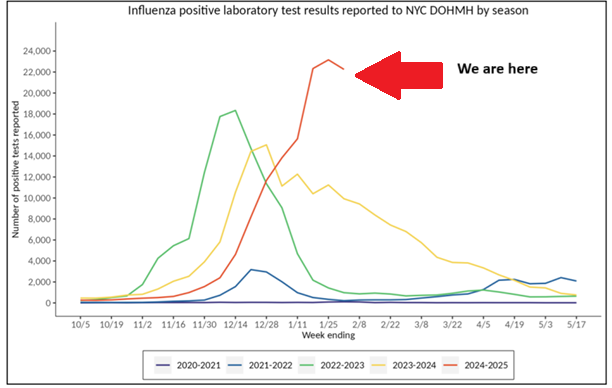
The H5N1 avian flu outbreak in the United States has been a sobering reminder of the pandemic potential lurking within zoonotic diseases. While the Centers for Disease Control and Prevention (CDC) maintains that the current risk to humans remains low, the year 2024 saw 66 confirmed human infections—most linked to infected cows or poultry, with two cases of unknown exposure sources.
Each infection represents a gamble, offering the virus an opportunity to mutate in ways that could enhance its ability to spread efficiently between humans, potentially triggering a larger epidemic. The outbreak also recorded its first fatal human case in Louisiana, where the patient, exposed to a sick backyard flock, developed a severe infection with concerning mutations. These mutations could enhance the virus’s ability to bind to human upper airway receptors, a development that underscores the need for vigilance.
Thankfully, efforts to mitigate a larger epidemic are well underway. States like California have declared emergencies to expedite their responses, and the U.S. Department of Agriculture (USDA) has launched the National Milk Testing Strategy (NMTS), which builds on measures taken since H5N1 was detected in dairy cattle in March 2024. Additionally, the Department of Health and Human Services (HHS) has allocated $306 million to bolster monitoring and preparedness efforts against H5N1.
Earlier this year, I co-authored an article outlining the critical role hospitals play in preparing for H5N1 and led one of the nation’s first full-scale healthcare system exercises on H5N1 preparedness. As an infectious disease epidemiologist and a leader in healthcare biopreparedness, I understand the urgency of these proactive measures to prevent and prepare for potentially calamitous outcomes, and it is encouraging to see such decisive steps being taken.
4. A Landmark Step in Environmental Health: Regulating PFAS in Drinking Water
The Biden-Harris Administration’s first-ever national drinking water standard for PFAS, or “forever chemicals,” marks a transformative moment in public health and environmental stewardship. Announced in April 2024, the Environmental Protection Agency’s (EPA) legally enforceable rule sets strict limits on toxic PFAS in drinking water, including PFOA and PFOS, at 4 parts per trillion—the lowest level reliably measurable.
This regulation, part of the EPA’s PFAS Strategic Roadmap, is expected to reduce exposure for 100 million people, prevent thousands of deaths, and significantly lower rates of serious illnesses, such as certain cancers as well as liver and heart conditions. Complementing this rule, the Biden Administration allocated $1 billion through the Bipartisan Infrastructure Law to help communities implement PFAS testing and treatment, part of a historic $9 billion investment to combat PFAS pollution.
The regulation addresses a critical public health challenge, as PFAS contamination has long plagued communities across the United States. These chemicals, commonly found in everyday products like nonstick cookware, firefighting foam, and waterproof clothing, persist in the environment and accumulate over time, leading to adverse health risks. My previous collaboration with a chemist colleague highlighted PFAS exposure pathways, including general exposure (via drinking water, food, and household products), occupational exposure, and prenatal exposure, where contaminated umbilical cord blood crosses the placenta.
The EPA’s decisive action not only sets a new standard for water safety but also exemplifies the importance of a whole-of-government approach to environmental justice. While water utilities face challenges in implementing these measures, this landmark regulation underscores the value of prioritizing health, equity, and the environment to protect current and future generations from the harms of PFAS.
5. Combating Vaccine Mis and Disinformation: The “Let’s Get Real” Campaign
The launch of the HHS’s Let’s Get Real campaign marked a critical step in countering vaccine misinformation and disinformation, a growing threat as vaccination rates in the U.S. continue to decline. In the 2023–2024 school year, national vaccination coverage for key vaccines, such as measles, mumps, and rubella (MMR), fell below 93%, a concerning drop from the pre-pandemic rate of 95%. Additionally, 3.3% of U.S. kindergartners had exemptions from at least one vaccine, the highest rate ever recorded, with 14 states exceeding a 5% exemption rate. These alarming trends jeopardize herd immunity and heighten the risk of outbreaks of vaccine-preventable diseases.
HHS’s Let’s Get Real campaign arrives at a time when public rhetoric around vaccines remains polarized, shaped by misinformation and shifting attitudes toward routine immunizations. This shift also stems from hesitancy about COVID-19 vaccination or objections to vaccine mandates, fueling potential declines in coverage and rising exemptions. A 2024 survey revealed that 8.3% of U.S. parents disagreed with the necessity of school vaccination requirements, while 15.2% expressed no opinion, reflecting a troubling erosion of confidence in vaccines.
Campaigns like Let’s Get Real are critical to reversing these trends and rebuilding public trust in immunization. This mission aligns with my platform, Critical Health Voices, which seeks to amplify perspectives from frontline healthcare and public health experts to combat mis and disinformation and foster informed decision-making. Addressing falling vaccination rates demands a multi-faceted approach, including robust public health campaigns, strict enforcement of school vaccination requirements, and enhanced access to immunization services to ensure preventable diseases do not resurge.
The Road Ahead
While these accomplishments give us cause for celebration, they also highlight the persistent inequities and vulnerabilities that demand our attention. The lessons of 2024 reinforce the importance of preparation, innovation, and collaboration. They also remind us of the power of hope—hope that arises when science, policy, and humanity converge to protect and promote health.
As we look to 2025, I remain optimistic about the path forward. The successes of this year remind us that progress, while often hard-won, is achievable when we work together with purpose and determination.
Stay connected with Dr. Madad:
Instagram
Twitter/X
LinkedIn
Facebook
More from Dr. Madad on the Academy Blog
Dr. Madad’s Critical Health Voices on Substack