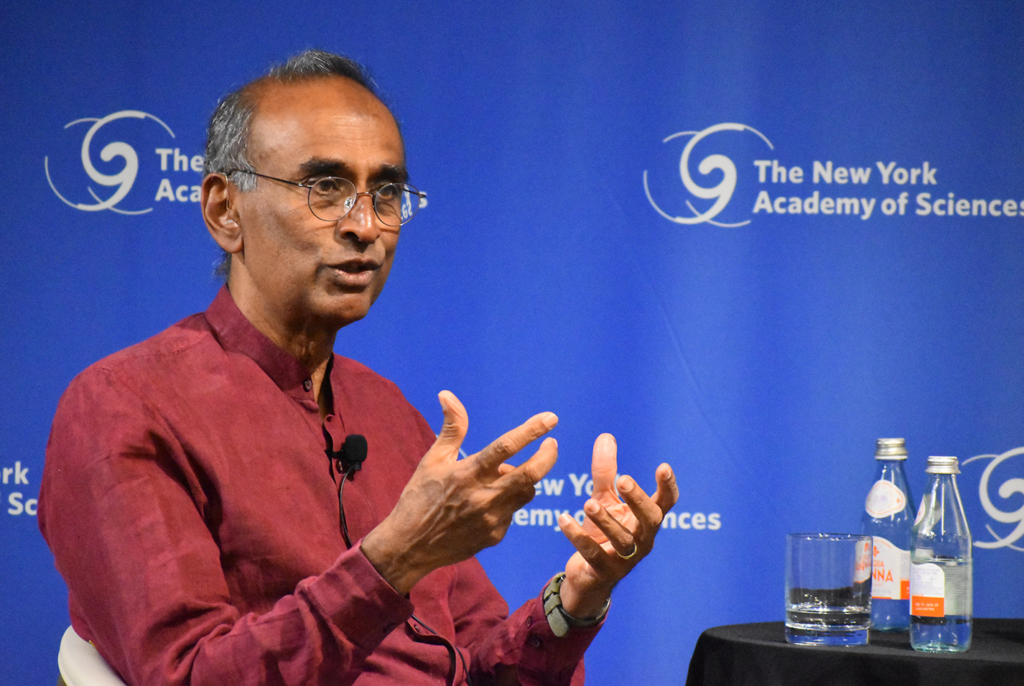
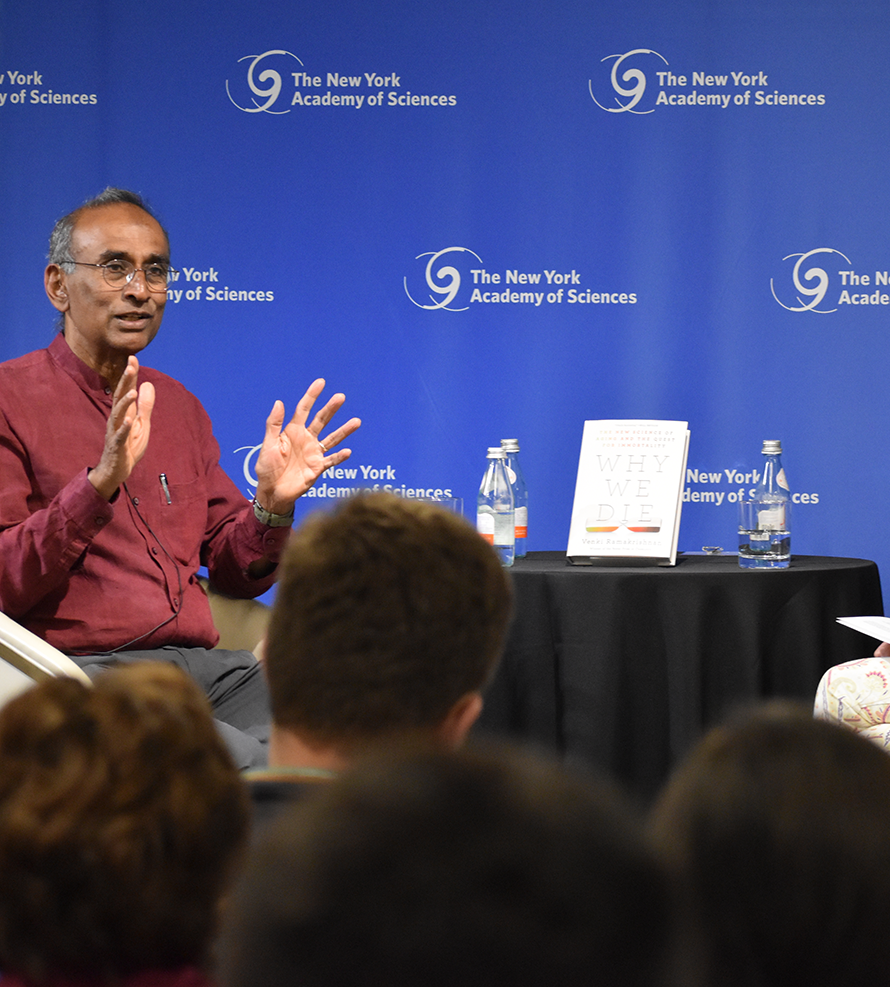
Nobel Laureate Venki Ramakrishnan, world-renowned molecular biologist, presents the science about why humans die.
Published May 7, 2024
By Nick Fetty

Why do we die? This age-old question is the topic of Nobel Prize-winning author Venki Ramakrishnan’s book Why We Die: The New Science of Aging and the Quest for Immortality.
Ramakrishnan discussed his new book with Titia de Lange, Director of The Rockefeller University’s Anderson Center for Cancer Research, during the “Authors at the Academy” event at The New York Academy of Sciences on April 16, 2024. He began by suggesting that humans may be the only species aware of its own mortality.
While societies have long focused on both the philosophical and the scientific dimensions of mortality, Ramakrishnan pointed out that aging research was considered “something of a backwater in molecular biology for a long time.” It’s only been over the past half-century that this field of research has become more mainstream.
“[While there have been advances in the research], because this is an area that people are concerned about, and they’re anxious about, there’s also a lot of hype,” said Ramakrishnan, who is also a member of the Academy’s President’s Council.
As a molecular biologist, Ramakrishnan avoided speculation, focusing instead on researching an objective, scientifically-based case about aging and mortality.
Evolution and Mortality
Ramakrishnan said there is a wide range in lifecycles of different creatures, from a mayfly which can live for just a day, to certain species of sharks and whales that may live for more than a century.
“A giant tortoise might be around today that could have encountered [Charles] Darwin,” Ramakrishnan said, with a nod to the renowned evolutionary biologist who was an honorary member of the Academy more than a century ago.

Researchers believe that evolution is largely focused on fitness, which, in this context, Ramakrishnan defined as “maximizing the ability to successfully pass on your genes.” Part of this fitness is tied to physical size. He pointed out that creatures like mice tend to have shorter lifespans than an elephant or a whale.
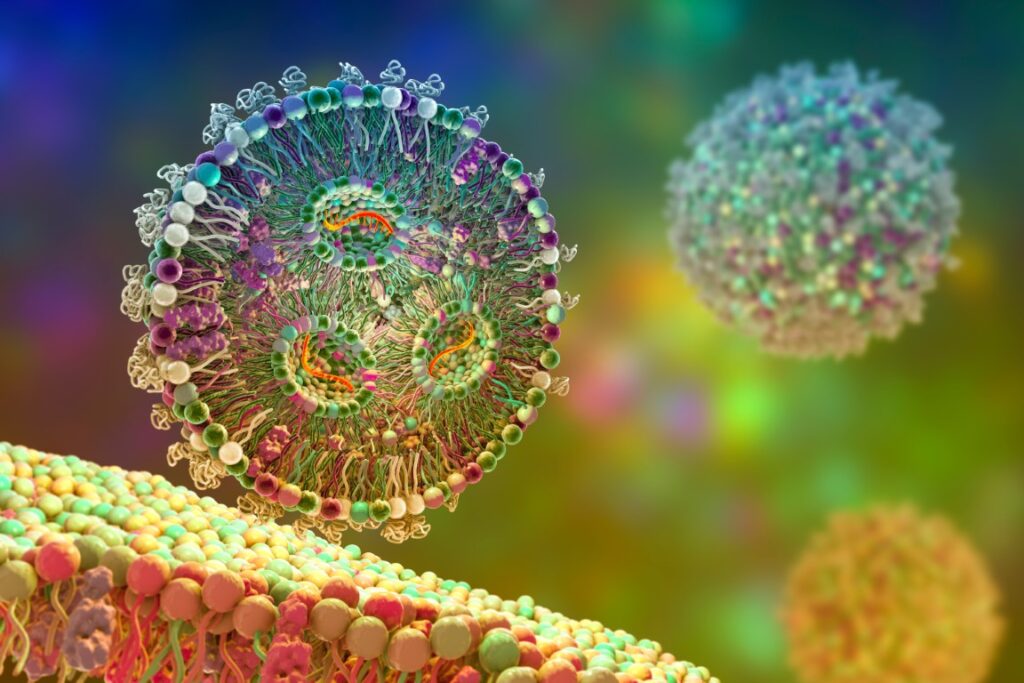
“You might ask, why is that?” Ramakrishnan said. “Well, aging is an accumulation of chemical damage which manifests itself from the molecular level all the way to the entire organism. To repair such damage takes lots of resources and lots of energy. So, this has a cost because animals are always trying to get energy.”
From an evolutionary standpoint, to maximize fitness it’s more advantageous for a creature like a mouse to allocate its resources to features such as rapid growth, rapid maturation, and producing many offspring. Conversely, larger animals allocate resources to repairing and maintaining natural chemical damage because such creatures need to live longer to raise their offspring to full maturity, Ramakrishnan argued.
This is what evolutionary biologists call the Antagonistic Pleiotropy theory. Based on this theory, genes that involve rapid growth or rapid maturation often turn out to be detrimental later in life and contribute to aging.
The Metabolic Rate Theory of Aging
According to Ramakrishnan, the metabolic rate theory states that “if you have increased metabolism then you’re generating byproducts…like free radicals and reactive species which can cause damage. So, the faster your metabolism is, the more likely the higher the rate at which you’re going to age.”
Generally, a faster metabolism means a shorter lifespan, but Ramakrishnan said this is not always the case. He used the example of some species of smaller bats, that are similar in size to mice, but because of the bat’s ability to fly, are less likely to be targets of predators, and can live for as long as 40 years.
“I think biologists would say it’s really about evolutionary choice and how each species has been selected for optimizing that choice,” said Ramakrishnan. “That choice could be, yes there’s damage but you can also repair the damage, so how much do you spend on repairing the damage?”
Researchers who study aging are divided about the potential maximum lifespan of humans. Some believe that 115 is the top of the range, while others feel that the first person to live to 150 has already been born. Ramakrishnan said he thinks the current natural limit is around 120 years, citing the fact that the number of centenarians (those who live to the age of 100) has increased in recent decades, but the number of people who live past the age of 110 has not.
“That suggests that those people who reach 110, are hitting some natural limit of our biology, of our species,” said Ramakrishnan, adding that he feels that those who think the upper limit is 150 are being “excessively optimistic.”
Societal Impacts of Expanded Lifespans

Science aside, what are the societal impacts of expanded lifespans? Several private sector tech billionaires have shown interest in extending lifespans. As Ramakrishnan points out, the issue has also been on the radar of government agencies such as NIH’s National Institute on Aging in the US or the Medical Research Council in the UK.
“So, the question is how do we keep people healthy for as long as possible so people can stay productive?” asked Ramakrishnan.
The answer may well lie with the next generation of scientists who will bring in innovative ideas and fresh perspectives. While Ramakrishnan remains productive, he concedes it may be time to retire next year.
“I think there are lots of roles we can play without taking away resources from the younger people,” said Ramakrishnan, citing examples like serving on editorial boards or as mentors. “Generational turnover is good for society and good for science.”
For on-demand video access to the full event, click here.
Check out the other events from our 2024 Authors at the Academy Series
- Reid Hoffman – Impromptu: Amplifying Our Humanity Through AI
- Erika Nesvold – Off-Earth: Ethical Questions and Quandaries for Living in Outer Space
- Claudia de Rham – The Beauty of Falling: A Life in Pursuit of Gravity
- Arthuro Casadevall – What if Fungi Win?
Full video of these events is available, please visit nyas.org/ondemand