A recent Academy event explored near-death experiences and the medical application of psychedelic remedies, combining elements of science and philosophy.
Published June 9, 2023
By David Freeman
What is the nature of consciousness? What happens to it at the brink of death—and beyond? In what ways can the scientific study of near-death experiences and the medicinal use of psychedelic compounds boost our understanding of the human condition and our ability to ease emotional suffering?
These and related questions were the focus of an Academy conference held on June 8, 2023, in New York City. The one-day event included presentations by psychologists, neurologists, biomedical researchers and a religious scholar. Additionally, there was a gripping first-person account of a near-death experience from renowned journalist and author Sebastian Junger.
What are Near-Death Experiences?
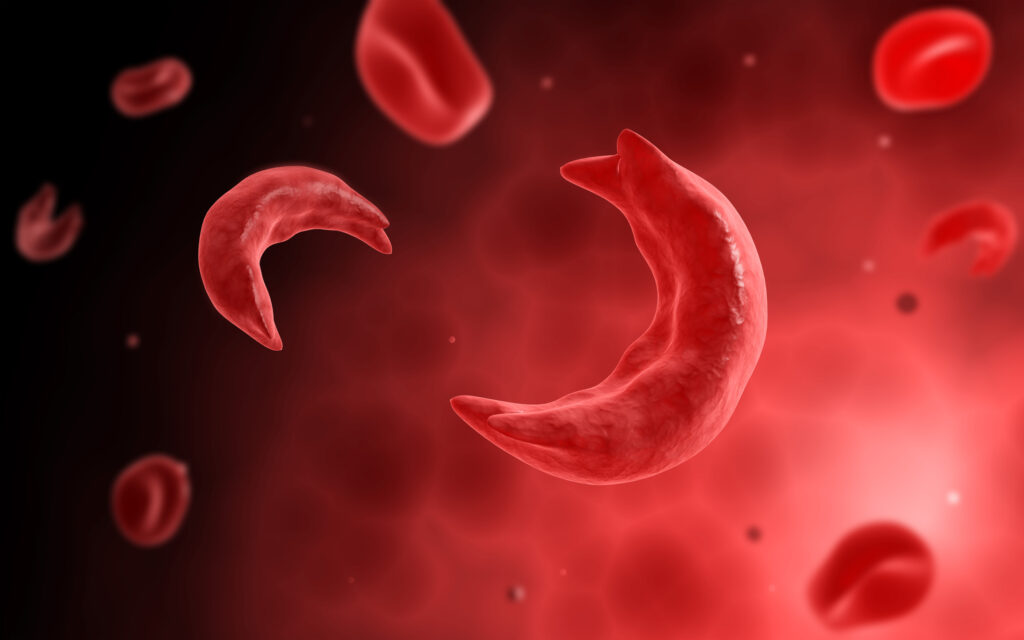
Near-death experiences, or NDE’s, are deeply affecting, often mystical episodes. Experts call them periods of “disconnected consciousness.” They affect some people who are close to death or in situations of grave physical or emotional danger. They are commonly marked by feelings of floating outside one’s body and the sensation of moving toward a bright light, as well with as encounters with dead relatives.
NDE’s have been documented across many different cultures and have been known since ancient times. “We’re talking about something that could be hundreds of thousands of years old,” said Brian C. Muraresku. He is the author of the 2020 book “The Immortality Key.” His book examines scientific evidence for the ritual use of psychedelics in classical antiquity. He was also one of the speakers at the conference.
There’s something about that kind of experience—near-death, psychedelic, mystical, whatever it is—that holds the entire human race together.
Brian C. Muraresku, author “The Immortality Key”
NDE’s are now known to be remarkably common. In recent research, 15 percent of intensive care unit patients reported having one. As did up to 23 percent of survivors of cardiac arrest. This is according to neuropsychologist Helena Cassol, Ph.D. Dr. Cassol is the scientific coordinator of Neurological Rehabilitation Center of the University Hospital of Liege in Belgium and also presented at the conference.
“More people have survived cardiac arrest and other situations and could recall those experiences” as a result of improved resuscitation techniques that have become available in recent years, she explained. She added that NDE’s now represent an emerging field of scientific research.
NDE’s can be personally transformative. Some people report a reduced fear of death in the wake of an NDE. Others report enhanced feelings of compassion or purpose. But some are saddled with a pattern of persistent intrusive thoughts or dreams or other negative after-effects. Given these possibilities, “I think it is important for people to be able to talk about these experiences and be heard in a nonjudgmental way,” Dr. Cassol said.
The Evolution of Near-Death Experiences
There may be an evolutionary basis for NDE’s. Daniel Kondziella, M.D., Ph.D., is a neurologist at Copenhagen University Hospital and an associate professor at the University of Copenhagen in Denmark. During his conference presnetation he described research linking the episodes to thanatosis. That’s the well-documented and remarkably consistent phenomenon in which animals—even insects—feign death in order to avoid being killed by predators.
The research suggests that the evolution of language in humans gave us the unique ability to transform this stereotyped behavior into the rich narratives used to describe the mysterious sensations and perceptions commonly seen in near-death experiences, Dr. Kondziella said. Not everyone is convinced by such research.
“Evolutionary explanations are just-so stories,” said Christof Koch, Ph.D. Dr. Koch is chief scientist and president of the Allen Institute for Brain Science, and also presented at the conference. “They may be true. They made be false. It just doesn’t matter. But the fact that we do have experiences—that is the remarkable thing.”
Studies of the neurological underpinnings of NDE’s suggest that the phenomenon arises amid a sort of blending of conscious states: waking, rapid-eye movement (REM) sleep and non-REM sleep.
“The physiological balance between conscious states is disrupted during the conditions of near-death, leading the brainstem arousal system controlling conscious states to blend waking and rapid eye movement consciousness into a hybrid state” known as REM intrusion,” said Kevin R. Nelson, M.D., a University of Kentucky neurologist and another speaker at the conference. “REM intrusion leads to many key features of near-death, including lying still, visual activation, out-of-body, and the experience’s narrative qualities.”
Most individuals who experience near-death are physiologically predisposed to REM intrusion, according to Dr. Nelson.
Psychedelics as Medical Treatment
As some scientists work to gain a better understanding of NDE’s, others are pursuing clinical trials of psychedelic compounds, which have been shown to trigger an altered state of awareness similar to that seen in people experiencing an NDE. A growing body of evidence suggests that these compounds—given under expert supervision and in carefully controlled settings—can ease emotional distress in terminally ill people quite profoundly.
One landmark 2016 study by researchers including Anthony P. Bossis, Ph.D., clinical assistant professor of psychiatry at NYU Grossman School of Medicine and another speaker at the conference, showed that a single treatment with psilocybin—a psychoactive compound found in some mushroom species that humans have consumed for thousands of years—brought rapid reductions in depression, anxiety, and hopelessness in people with terminal cancer.
The benefits of psilocybin treatment were greatest among individuals who reported strong mystical experiences during the sessions, according to Dr. Bossis. “The more robust that mystical experience, the greater the outcome in terms of reduction of depression,” he said. “These aren’t NDE’s,” he added, “but they’re deathlike experiences with a similar phenomenology.”
Recent research shows that psilocybin is just one of many drugs that can induce NDE-like such experiences and suggests that those induced by ketamine, an anesthetic with hallucinogenic effects, show greater similarity to NDE’s than those induced by psilocybin. But “we only studied the phenomenological similarity between subjective experiences” and didn’t assess the extent to which any of the drugs might be effective treatments for depression, said Charlotte Martial, Ph.D., a neuropsychologist at the University of Liege in Belgium and another conference speaker.
Junger’s Brush with Death
Sebastian Junger’s brush with death came three years ago, following the rupture of an aneurysm in his pancreatic artery. As doctors rushed to stanch the bleeding that threatened his survival, he recalled, he encountered an “infinitely dark” pit that threatened to pull him in but also the welcoming “essence” of his beloved, long-dead father. “It wasn’t quite a vision. It was halfway between a vision and a feeling,” he said.
A self-described atheist whose father was a physicist, Junger said the experience nonetheless led him to reconsider his ideas not only about life and death but about the nature of the universe.
“I wish I could say I believe in an afterlife. I don’t. But I definitely have lost the certitude of my rationality,” he said, adding that he now believes it was possible that “some kind of energy or quantum phenomena” interacts with reality in ways we don’t understand.
If some see NDE’s as possible evidence of the supernatural or a phenomenon beyond the scope of scientific knowledge, others are convinced that they are simply the result of physiological processes—such as the oxygen starvation to the brain that can result from cardiac arrest.
There is a “perfectly natural explanation for NDE’s,” said Dr. Kondziella. “No need to postulate any supernatural events.”
But Raymond A. Moody, Jr., M.D., Ph.D., the keynote speaker whose remarks set the stage for the conference, expressed uncertainty over what near-death experiences actually represent.
Science? Or philosophy?
“I really just don’t know,” he said. “I think the questions that we are dealing with—a lot of them are not yet scientific questions,” he added. “They are philosophical questions.”
Dr. Moody is the author of the 1975 book “Life after Life” that sparked interest in near-death experiences. He has been documenting NDE’s for many years and is credited with coining the term near-death experience.
Uncertainty about life’s transcendent questions is inevitable, according to Karen Armstrong, a London-based author of numerous books on religious affairs and the other keynote speaker at the conference.
“Neither religion nor science can really respond. Ultimately, we are all in a ‘Cloud of Unknowing,’” she said in a reference to an anonymous 14th Century text on spirituality and Christian mysticism. “We are all just trying to find some meaning in it all,” she added, “without which we humans fall very easily into despair.”
For Brian C. Muraresku, the strange perceptions and complex emotions seen in near-death and similar visionary experiences are central to the human experience. “There’s something about that kind of experience—near-death, psychedelic, mystical, whatever it is—that holds the entire human race together.”
Also read: Music on the Mind: A Neurologist’s Take