By utilizing an individual participant data meta-analyses, researchers were able to shed new light on prenatal multiple micronutrient supplementation.
Published September 24, 2025
By Nick Fetty

A multi-year research project by The New York Academy of Sciences’ Nutrition Science Program has resulted in promising findings for positive birth outcomes based on when supplementation is started during pregnancy and how consistently it’s taken.
Findings from the project were published in the July issue of Advances in Nutrition. The international team of researchers assessed the impact of timing of initiation and adherence on the effectiveness of multiple micronutrient supplements (MMS). The researchers conducted a two-stage individual participant data meta-analysis that included 15 randomized trials with 61,204 pregnant women.
The findings showed that higher adherence to MMS was consistently linked to better birth outcomes, highlighting the importance of early initiation and program strategies that support sustained use. For example, women who had adherence to MMS of 90% or better had babies that were on average 56 grams heavier than those who took iron and folic acid alone, and the risk of delivering babies with low birthweight (i.e. weighing less than 2.5 kilograms) was reduced by 12% in this high adherence group. On the other hand, those who took less than 60% of the supplements had no difference in birth weight.
“The Academy has been working on prenatal MMS since 2017,” said Filomena Gomes, PhD, a former program manager for the Academy’s Nutrition Science Program. “The expertise and network created since then enabled the coordination of this complex project with 37 co-authors.”
The Strength of an Individual Participant Data Meta-analysis
Part of what made this research different from similar, past projects is that it conducted an individual participant data (IPD) meta-analysis in a new way. The advantage of the IPD is that it provides the researchers with data from each participant in the trial.
“Other methods, such as the Cochrane reviews, use the averages from the trial so you lose a lot of detail and information,” said Megan Bourassa, PhD, the former Associate Director for Nutrition Science at the Academy. “For example, there was a wide range in the number of pills consumed in some trials, and we are able to parse that information, rather than relying on single data points from each trial.”
While IPD meta-analyses have been used in this field of research in the past, the approach on this project was different.
“Other individual participant data meta-analyses have been conducted previously to assess the benefits of prenatal MMS on various outcomes, but this is the first individual participant data meta-analysis to assess and examine the timing of initiation and adherence of MMS,” said Dr. Gomes.
A Team Effort
The researchers gave special acknowledgement to the efforts of all 15 of the trial groups. These trial groups either provided raw data or analyzed their previously collected data based on this project’s protocol. Support was also provided by JBJ Foundation, a non-profit organization focused on the “most cost-effective ways to create impact for the world’s poorest.”
The Academy partners with other organizations to explore solutions across the nutrition spectrum. By convening diverse groups, synthesizing evidence, building consensus, designing roadmaps, and preparing scientific manuscripts for publication, the efforts build solutions that use nutrition science to support and advance public health.
“This work is important for implementing supplementation programs for pregnant women in low- and middle-income countries because we can now show how much starting early and taking it consistently matters for the health of the mother and baby,” Dr. Bourassa said.
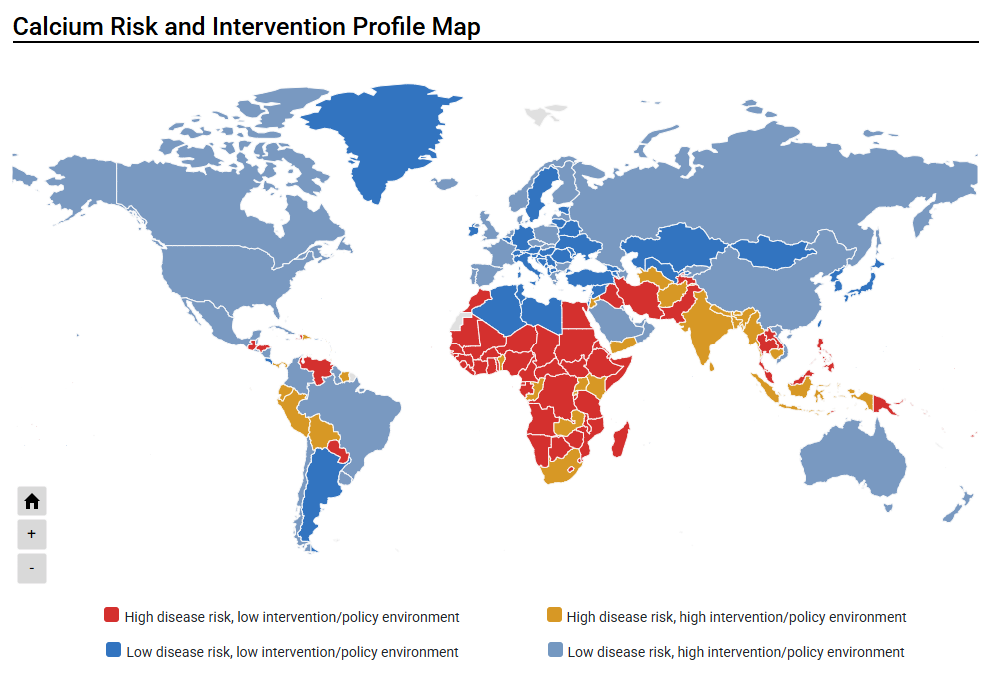
Also read: A Multidisciplinary Approach to Address Inadequate Calcium Intake